Using 3D cancer cell models to push forward personalized medicine
Using 3D cancer cell models to push forward personalized medicine: an interview with Angeline Lim, PhD, of Molecular Devices
Editor-in-Chief, Francesca Lake, speaks to Angeline Lim of Molecular Devices about using 3D cancer cell models to inform the future of precision medicine.
What are some of the main challenges in designing effective cancer treatments?
A central challenge is that every cancer is different, so a medication that effectively treats one patient may not work for the same type of cancer in another. But even within an individual, cancer that derives from a single cell can mutate or change over time, contributing to drug resistance. Thus, a single therapy may not be sufficient for all of the cancer cells within one individual. Sometimes a tumor will reduce in size with treatment, but certain cells may grow more aggressively if they’re resistant to the prescribed drugs. Many cancer cells simply don’t die, often because they have some genetic mutation that we haven’t mapped out yet or they are unaffected by the prescribed drugs. This kind of variation within a tumor is known as clonal heterogeneity.
How can in vitro models lead to more personalized cancer care?
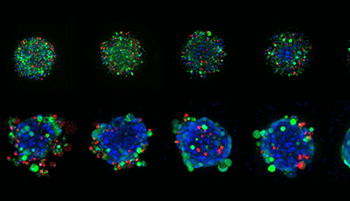
In vitro cell modeling is usually done using 2D models, such as animal models or cell cultures, in a petri dish. But 2D models have a number of drawbacks that make them less indicative of natural cancer cells in an organism. Yet when you culture in 3D using spheroids—a type of three-dimensional cell model that better simulates a live cell’s environmental conditions—you can get a much better sense of what’s actually happening to it within the body.
Interestingly, studies have shown that cells isolated from different parts of a tumor respond differently to the same drugs. A method to address this is to take tumor cells from an individual patient and transplant them into immune-deficient mice to grow. The resulting tumor can then be dissected and grown in 3D cultures to evaluate personalized drug responses. This so-called patient-derived xenograft (PDX) model has been known to sufficiently resemble the cellular heterogeneity within a patient’s tumor, and can be better used for identification of gene mutations to predict effective treatment approaches.